The Treatment of Androgenetic Alopecia with LLLT Devices (此为医学研究报告,只提供英文版本)
The Treatment of Androgenetic Alopecia with LLLT Devices
A Discussion of Industry Knowledge
Introduction
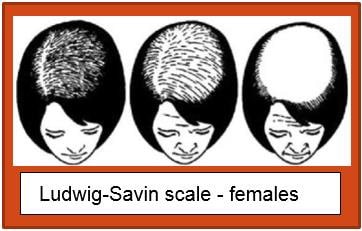
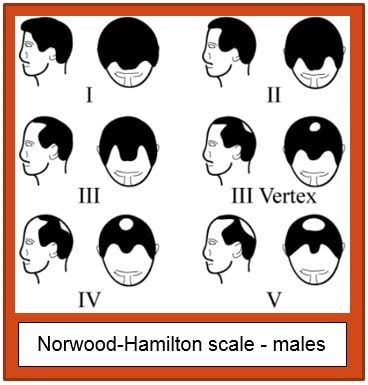
Low level laser (light) therapy (LLLT) has been well studied and is used clinically to treat a wide range of conditions including androgenetic alopecia. Several devices have received market clearance for the treatment of androgenetic hair loss and to promote hair growth in men with Hamilton-Norwood IIa-V and women with Ludwig-Savin I-II classifications of hair loss, and possessing Fitzpatrick I-IV skin types.
A widely accepted theory is that LLLT, particularly at wavelengths in the red (visible) range, affects the functioning of the stem cells that cause hair growth. LLLT activates cytochrome c oxidase and increases mitochondrial electron transport [11-17], which leads to an increase in ATP and subsequent reversal of hair follicles from the dormant telogen stage of growth, to the active growth or anagen stage [27, 28, 30-32,34, 35, 38].
This discussion will focus on the three areas significant to low level light therapy devices. First, the physical design and technical characteristics of the various devices; second, the clinical efficacy and safety risk assessment; and finally, the intended user population.
| Name | Wavelength |
|---|---|
| Gamma Ray | < 0.01 nm |
| X-ray | 0.01 nm – 10 nm |
| Ultraviolet | 10 nm – 380 nm |
| Name | Wavelength |
|---|---|
| Visible | 380 nm – 700 nm |
| Infrared | 700 nm – 1 mn |
| Microwave | 1 mn – 1 meter |
An optical designer may provide a scientific basis for adopting any of the above variables in a specific format, in order to deliver an effective fluence. The iGrow-II Hair Growth System, which is hat shaped and has 51 light elements (including LEDs), the HairMax laser comb, which is a “brush” shaped device with up to 82 lasers, and the Sunetics which does not specify the number of elements, only the shape of the layout (“flat, open panel”) are examples of the variability of characteristics, which still deliver treatments in a way that the FDA considers substantially equivalent to the first device cleared. All of the devices cleared by the FDA for the specific purpose of treating androgenetic alopecia and promoting hair growth are operating in the visible light range; specifically at or around 650 nm.
THE PHYSICAL DESIGN DOES NOT SEEM TO AFFECT EFFICACY, UNLESS WE CONSIDER, FOR EXAMPLE, A DESIGN THAT WILL ENCOURAGE COMPLIANCE WITH THE REQUIRED REGIMEN DUE TO EASE OF USE AND/OR PORTABILITY.
Now that we are providing energy in the “right” wavelength for our purpose, let’s discuss energy delivery. Laser fluence is a measure used to describe the energy delivered per unit (or effective) area. Within the community of laser scientists and technicians it is very common to describe fluence in units of Joules per centimeter, squared (J/cm2). The important variables to consider when calculating fluence are 1) the shape of the beam (e.g. Gaussian, flat-top, semiconductor beam), 2) the distance to target, and 3) the duration of time the light is emitting (pulse width).
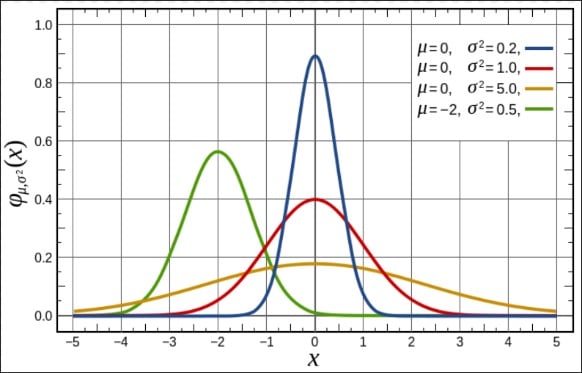 Figure 1: Gaussian Beam Profile
Figure 1: Gaussian Beam ProfileWithout delving into too much technical detail, the important thing to know about Gaussian beams is that the intensity of light is highest at point of origin. Consider Figure 1 to the left. The light is most intense at the peak of the curve, and loses intensity exponentially as it travels outward from the origin. This is a common shape for the output of laser diodes which commonly do not have focusing lenses.
Less common with laser diodes is a flat top beam profile (see Figure 2). As with the Gaussian distribution, the flat top is most intense at point of origin. To really confuse the matter, each diode will display distinct variances that are acceptable to a certain point.
Click to see Figure 3. Looking closely, neither Gaussian nor flat profiles are seen in reality, especially when the light source is a diode laser.
The behavior of laser light (unfocused) is to spread and penetrate until stopped, either by obstruction or by loss of impetus (force / intensity); in this case, a combination of both.
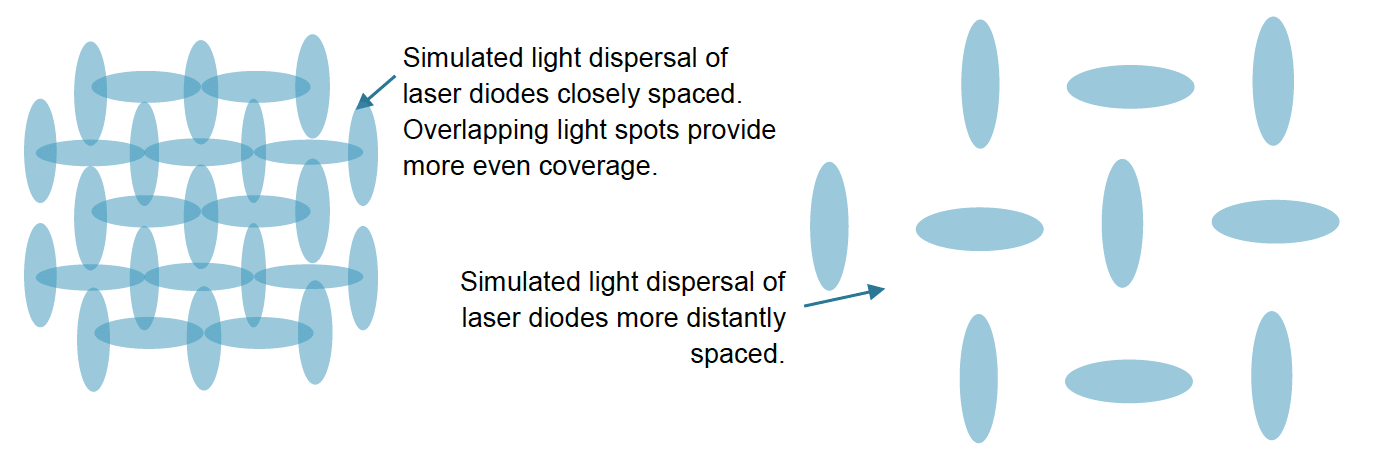
Figure 4: The beam is most intense at the point of origin, and loses intensity as it travels down and spreads to surrounding cells. If the diodes are placed far apart, the coverage is not as efficacious as with much closer spacing. In the top layer of the skin, the cells get relatively high power density, while cells situated beside the aperture and lower down receive a relatively low density of light. Consider the arrays below. There is a lot of overlap (resulting in more even coverage) with closely spaced diodes.
Therefore, in addition to distance from target, we must also considerdistance between laser diodes.
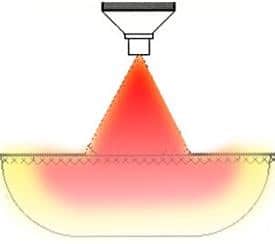 Figure 4: Typical beam spread
Figure 4: Typical beam spreadThe Capillus272 Pro contains 272 light elements or about 5 times as many as some other portable devices. The clinical study results for the Capillus272 Pro indicated a 51% increase in terminal hair growth for the users of the active device over the results of the placebo group. Capillus’ optical designer postulates that more light elements may lead to increased efficacy due to coverage (little to no gaps in light coverage).
Indications for Use, Regimen, and Risks of Use
We continue our discussion by addressing user risks, the indications for use, and demonstration of efficacy achieved through clinical testing.
Specific safety concerns, such as eye exposure to intense light, associated with visible light devices such as these are negligible; especially when accompanied by safety interlocks to limit eye exposure. Regulations (e.g. 21 CFR 1040.10) specify the required safety and cautionary labeling and that such labeling shall be prominently placed (for some light-based devices the exact spot is specified). User instructions accompanying the Capillus272 Pro stipulate to operate the device only when situated correctly on the head. An integrated safety interlock pauses treatment if the cap is not situated correctly.
Many of the portable devices are compliant with SELV (safety extra-low voltage) requirements, which carries a negligible risk of injury associated with electricity or heat. In fact, the requirements for LLLT include the voltage output of the light diode be ≤ 5mW. The output voltage, wavelength, and pulse width (time of exposure) all contribute to fluence (delivered light energy). Thus, when limited in one variable (output voltage), an optical designer will adjust the other variables (wavelength and pulse width) to obtain the optimal light density for treating hair loss and promoting hair growth. Wavelength is also limited within a small range; therefore, the variable to concentrate on is pulse width, or the time the light pulse remains on, and how long it remains off. One independent variable remains – number of diodes and placement in an array as discussed above.
Functionally, there is no question that the intended use, regimen, and technology are the same across all current devices (see Table 1). All contain class IIIa/3R laser diodes (or equivalent LEDs) and all employ the same (or very similar) user regimen and indications for use. There may be a question of equivalent delivery of energy to the target tissue, i.e., the human scalp, because the number of diodes varies from device to device. Although each diode will deliver energy similar to other diodes of the same technical specifications (e.g. ≤ 5mW + similar pulse width = similar fluence), the number of diodes and the geographical array may make a difference to efficacy with regard to coverage.
Key points:
- All systems are products that form a group of devices called Low-Level Laser/Light Therapy devices.
- All systems contain semiconductor laser diodes and/or LEDs that operate at a similar wavelength for visible red light from the Electromagnetic Spectrum.
- All systems have the same IEC (International Electrotechnical Commission) classification for laser products – Class IIIa/3R
- All systems have the same safety and adverse effect profile.
- All systems have the same Common Name – Lamp, non-heating for promotion of hair growth.
- All systems have similar treatment protocols – 3-4 times per week on non-consecutive days for 16 – 26 weeks (to see noticeable first results; to maintain results, the device is intended to be used indefinitely).
| PRODUCT | COMPANY | APPROVAL DATE | 510(K) NUMBER | Product Code |
|---|---|---|---|---|
| Capillus82 | Capillus, LLC | 08/21/2015 | K151516 | OAP |
| Lasercap LC pro and LC Elite18 | Transdermal Cap, Inc. | 07/22/2015 | K150613 | OAP |
| Capillus272 OfficePro | Capillus, LLC | 6/9/2015 | K150578 | OAP |
| LX-100 Hair Growth Stimulation System | Hairlabs International, Inc. | 4/14/2015 | K142824 | OAP |
| Capillus272 Pro | Capillus, LLC | 1/29/2015 | K143199 | OAP |
| NUTRA STIM LASER COMB | NUTRA LUXE MD LLC | 1/8/2015 | K141588 | OAP |
| NUTRA STIM LASER COMB | NUTRA LUXE MD LLC | 1/8/2015 | K141596 | OAP |
| IGROW II HAIR GROWTH SYS | APIRA SCIENCE INC. | 12/5/2014 | K140931 | OAP |
| HairMax LaserComb | LEXINGTON INTERNATIONAL LLC | 12/1/2014 | K142573 | OAP |
| IGROW / IGROW II HAIR GROWTH SYS | APIRA SCIENCE INC. | 8/21/2014 | K141567 | OAP |
| SUNETICS CLINICAL BIO-STIM LASER | SUNETICS INTERNATIONAL LLC | 12/20/2013 | K132646 | OAP NHN |
| LASERBRUSH | SUNETICS INTERNATIONAL LLC | 6/27/2013 | K121920 | OAP |
| LASER HELMET | THERADOME INC. | 6/14/2013 | K122950 | OAP |
| IGROW II HAIR GROWTH SYS | APIRA SCIENCE INC. | 12/5/2012 | K122248 | OAP |
| LASER HELMET | THERADOME INC. | 3/2/2012 | K113097 | OAP NHN |
| HAIRMAX LASERCOMB | LEXINGTON INTERNATIONAL LLC | 9/26/2011 | K112524 | OAP |
| HAIRMAX DUAL 12 | LEXINGTON INTERNATIONAL LLC | 8/16/2011 | K111714 | OAP |
| HAIRMAX LASERCOMB | LEXINGTON INTERNATIONAL LLC | 5/27/2011 | K110233 | |
| HAIRMAX LASERCOMB | LEXINGTON INTERNATIONAL LLC | 4/6/2011 | K103368 | OAP |
| E-LIGHT LINE | ESPANSIONE MARKETING S.P.A | 9/20/2010 | K092734 | GEX ISA OAP |
| MEP-90 HAIR GROWTH SYSTEM | MIDWEST R.F. LLC. | 2/23/2010 | K091496 | OAP |
| HAIRMAX LASERCOMB | LEXINGTON INTERNATIONAL LLC | 11/23/2009 | K093499 | OAP GEX |
| HAIRMAX LASERCOMB | LEXINGTON INTERNATIONAL LLC | 1/18/2007 | K060305 | OAP |
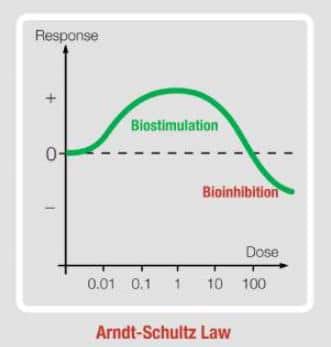 Figure 5: Arndt-Schultz Law
Figure 5: Arndt-Schultz LawThis brings us to a discussion of Arndt-Schultz Law (Figure 5), which claims: For every substance, small doses stimulate, moderate doses inhibit, and large doses may terminate life processes. With low-level laser therapy, we strive to accomplish biostimulation; defined here as the “small” dose. If we raise the intensity of light delivered (significantly), the result is permanent hair removal; think of this as the “large” dose. Alternatively, when a user thinks that more frequent or longer treatments will yield better results; it is in fact, the opposite; however, the result is not permanent (at least not in the short term). To complete our example, the latter would be the “moderate” dose. Thus, there is specific instruction by manufacturers of LLLT devices; that is:
Follow the use instructions! Do not use more often or for longer periods than prescribed!
A study conducted by a neutral third party for Capillus, LLC, demonstrates that low level laser treatment of the scalp every other day for 17 weeks using the Capillus272 Pro device is a safe and effective treatment for androgenetic alopecia. ClinicalTrials.gov Identifier: NCT01967277. Subjects receiving LLLT at 650 nm achieved a 51% increase in hair counts as compared to sham treated control patients. Active Treatment Group Subject Pre and Post Treatment Images are presented in Figures 6 and 7.
HAIR COUNTS FOR SUBJECT A WERE 39 AT BASELINE AND 87 POST TREATMENT. HAIR COUNTS FOR SUBJECT B WERE 97 AT BASELINE AND 153 POST TREATMENT.
Figure 6: A 53 year-old Caucasian female, Fitzpatrick skin phototype III, Ludwig-Savin 1-3, with a history of androgenetic alopecia. This subject was enrolled into the active test device group. After 17-weeks of compliant home use treatments, she returned for her final photography and release from the trial.
Primary Response
The formatted photographs were submitted for terminal hair counting. In the pre-treatment image, 39 terminal hairs were counted. In the post-treatment image 87 terminal hairs were counted. This demonstrates a 123% increase in terminal hairs from baseline.

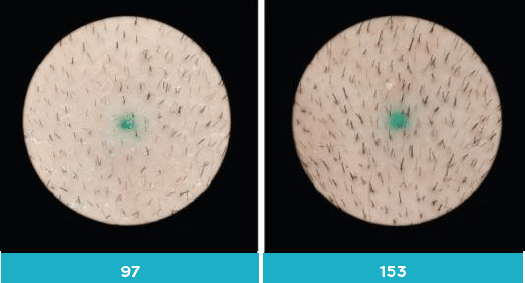
Figure 7: A 49 year-old Caucasian female, Fitzpatrick skin phototype II, Ludwig-Savin 1-1, with a history of androgenetic alopecia. This subject was enrolled into the active test device group. After 17-weeks of compliant home use, treatments she returned for her final photography and release from the trial.
Primary Response
The formatted photographs were submitted for terminal hair counting. In the pre-treatment image, 97 terminal hairs were counted. In the post-treatment image 153 terminal hairs were counted. This demonstrates a 57% increase in terminal hairs from baseline.
Are Men and Women Created Equal?
The final part of this discussion focuses on gender; specifically, the question whether there is a difference between men and women with regard to the physical function of hair regrowth. This investigator could find no published empirical evidence or reference regarding hair regrowth as a gender specific function, other than pattern; i.e. the form in which hair is lost. We could find no scientific paper postulating that there is a difference in the physical function of hair growth for men vs. that for women. Overall thinning is more prevalent in women, and “receding hairline” or “monk’s spot” are more common in men; however, for external strategies for regrowth (i.e. LLLT), there are no published differences in industry literature.
There is also a lack of published data specifically regarding the treatment (or difference in treatment) of androgenetic alopecia in women vs. men; this very lack of such discussion gives credence to the argument that there is no difference. The only discussions regarding gender are focused on the differences between the patterns of hair loss, and the increased likelihood with women that hair loss is attributable to reasons other than genetics.
Any reference to treatment difference between men and women is limited to the use of drugs and topicals which target specific hormones which do present differently between the genders. When asked, Dr. Shelly Friedman stated that with regard to low-level laser therapy, he prescribes essentially the same treatment regimen for men and women who present with androgenetic alopecia. Capillus LLC postulates this lack indicates there is no difference with regard to the physical function of hair regrowth, other than the normal differences found in individuals; that is to say, treatment regimen is adjusted by physician prescription based on each individual’s needs, not specific to gender.
Physicians use a system known as the Norwood-Hamilton Classification (men) and the Ludwig-Savin Scale (women) to describe the degree of hair loss. Devices cleared by the FDA for low level laser therapy are intended for promotion of hair growth in males who have Norwood Hamilton Classifications of IIa to V and in females who have Ludwig (Savin) I-4, II-1, II-2, or frontal patterns of hair loss and have Fitzpatrick skin phototypes I to IV.
This is the main reason Capillus LLC sells only to licensed health care providers rather than over the counter – to ensure the device is used by patients diagnosed with androgenetic alopecia and that these patients have medical advice with regard to optimal regimen.
In the clinical trials for LLLT devices reviewed for this paper, the treatment regimen between genders are the same. This also supports the premise that there is no difference between men and women with respect to the physical function of hair growth.
The following excerpts are intended to represent a consensus of available data
(References are listed at the end of this paper)
The [present study] demonstrates that that low level laser (light) treatment of the scalp every other day for 16 weeks using the [XXX] device is a safe and effective treatment for androgenetic alopecia in healthy women … with Fitzpatrick Skin Types I–IV and Ludwig–Savin Baldness Scale I-2–II-2 baldness patterns. Subjects … achieved a 37% increase in hair counts as compared to sham treated control patients. These results are similar to those reported in an earlier study using the same device in males with alopecia. [From the clinical results published for iGrow, K140931]
“Androgenetic alopecia (AGA), also known in women as female pattern hair loss, is caused by androgens in genetically susceptible women and men. The thinning begins between ages 12 and 40 years, the inheritance pattern is polygenic, and the incidence is the same as in men.”[40]
“In susceptible hair follicles, dihydrotestosterone (DHT) binds to the androgen receptor, and the hormone-receptor complex activates the genes responsible for the gradual transformation of large terminal follicles to miniaturized follicles. Both young women and young men with AGA have higher levels of 5 reductase and androgen receptor in frontal hair follicles compared to occipital follicles.”[40]
“Low level laser therapy is a safe form of light treatment used to treat the genetic forms of hair loss common in men and women, androgenetic alopecia or pattern balding.”[43]
Androgenetic alopecia can affect up to 70% of men (male pattern balding) and 40% of women (female pattern balding) at some point in their lifetime. While men typically present with a distinctive alopecia pattern involving hairline recession and vertex balding, women normally exhibit a diffuse hair thinning over the top of their scalps. [Various]
“Low level laser therapy (LLLT) uses devices with diodes that emit red light (wavelength range from 630-670 nanometers), and are available 1) in-salon hoods or overhead panels, 2) as bonnet or head caps, and 3) as hand-held devices.”[47]
“Low level laser therapy is intended for men and women with thinning hair or pattern baldness caused by a hereditary condition.”[49]
The hair growth cycle consists of three phases: growth (anagen phase), resting (telogen phase) and shedding (catagen phase). Hair loss in androgenetic alopecia depends on a testosterone derivative in the skin, dihydrotestosterone (DHT). Low level laser therapy is believed to increase blood flow in the scalp and stimulate metabolism in catagen or telogen follicles, resulting in the production of anagen hair. In theory: The photons of light act on cytochrome C oxidase leading to the production of adenosine triphosphate (ATP). This is converted to cyclic AMP in the hair follicle cells, releasing energy and stimulating metabolic processes necessary for hair growth. Release of nitric oxide from cells leads to increased vascularization to the scalp distributing nutrients and oxygen to the hair roots. Excessive build-up of DHT is prevented. [Various]
Laser hair therapy may be delivered in a salon by professionals trained in its administration, or at home. Two to three times weekly treatments are typically recommended, and consist of an 8 to 40-minute exposure of the scalp to light-emitting diodes under a bonnet or head cap or using a handheld comb or brush. [Various references to treatment regimens, paraphrased]
Conclusion:
Benefits of laser therapy for hair loss: 1) Low level laser therapy can be used in both men and women; 2) No adverse effects have been reported; and 3) It is clean and painless.
These results suggest that the emerging technology of Low Level Laser Therapy may play a potentially significant role in health care providers’ armamentarium for the disease Androgenetic Alopecia (AGA).
References
-
Tuner J., Rode L.: Laser Therapy. Clinical Practice and Scientific Background. Sweden: Grangesberg: Prima Books, 2002;
-
Hopkins J. T., McLodat T. A., Seegmiller J. G., Baxter G. D.: Low-Level laser therapy facilitates superficial wound healing in humans: A triple-blind, sham-controlled study. J Train. 2004; 39(3):223-229.
-
Schindl A., Schindl M., Schindl L. Successful treatment of a persistent radiation ulcer by low power laser therapy. J Am. Acad. Dermatol. 1997; 37(4): 646-648.
-
Schindl M., Kerschan K., Schindl A., Schon H., Heinzl H., Schindl L.: Induction of complete wound healing in recalcitrant ulcers by low-intensity laser irradiation depends on ulcer cause and size. Photoimmunol. Photomed. 1999; 15(1):18-21.
-
Mester E., Mester A. F., Mester A.:The biomedical effects of laser application. Lasers Med 1985; 5(1):31-39.
-
Lam S., Abergel R. P., Castel J. C., Dwyer R. M., Lesavoy M. A., Uitto J.: Laser stimulation of collagen synthesis in human skin fibroblast cultures. Lasers Life Sci. 1986; 1:61-77.
-
Conlan M. J., Rapley J. W., Cobb C. M.: Biostimulation of wound healing by low-energy laser irradiation. A review. J Clin. Periodontal. 1996; 23(5):492-496.
-
Hawkins D., Houreld N., Abrahamse H.: Low Level Laser Therapy (LLLT) as an Effective Therapeutic Modality for Delayed Wound HealiPg. N YAcad Sci. 2005; 1056:486-493.
-
Passarella S., Casamassima E., Molinari S., Pastore D., Quagliariello E., Catalano I. , Cingolani A.: Increase of proton electrochemical potential and ATP synthesis in rat liver mitochondria irradiated in vitro by helium-neon laser. FEBS Lett. 1984; 175(1):95-99.
-
Stadler I., Lanzafame R. J., Evans R., Narayan V., Dailey B., Buehner N., Nairn J. 0.: 830- nm irradiation increases the wound tensile strength in a diabetic murine model. Lasers Med 2001; 28(3):220-226.
-
Morimoto Y., Arai T., Kikuchi M., Nakajima S., Nakamura H.: Effect of low-intensity argon laser irradiation on mitochondrial respiration. Lasers Surg. Med. 1992; 15(2):191-199.
-
Yu W., Nairn J. 0., McGowan M., Ippolito K., Lanzafame R. J.: Photomodulation of oxidative metabolism and electron chain enzymes in rat liver Photochem. Photobiol. 1997; 66(6):866-871.
-
Karu, T. I.: The Science of Low Power Laser Therapy. London: Gordon and Breach Publ. l 998 ; pp. 14-33, 53-94, 95-121.
-
Karu, T. I.: Primary and Secondary Mechanisms of Action of Visible to near-IR Radiation on Cells. J Photochem. Photobiol. B. 1998; 49(1):1-17.
-
Vladimiorv IA, Klebanov G. I., Borisenko G. G., Osipov A. N.: Molecular and cellular mechanisms of the low intensity laser radiation effect. 2004; 49(2):339-350.
-
Eells J. T., Wong-Riley M. T., VerHoeve J., Henry M., Buchman E. V., Kane M. P., Gould
-
. J., Das R., Jett M., Hodgson B. D., Margolis D., Whelan H. T.: Mitochondrial signal transduction in accelerated wound and retinal healing by near-infrared light therapy. Mitochondrion 2004; 4(5-6):559-567.
-
Silveira P. C., Streck E. L., Pinho R. A.: Evaluation of mitochondrial respiratory chain activity in wound healing by low-level laser therapy. J Photochem. Photobiol. B. 2007; 86(3):279-282.
-
Brondon P., Stadler I., Lanzafame R. J.: A Study of the Effects of Phototherapy Dose Interval on Photobiomodulation of Cell Cultures. Lasers Surg. Med 2005; 36(5):409-413.
-
Karu T.I.: Low power laser therapy. In: Vo-Dinh T. (ed.): Biomedical Photonics CRC Press, 2003:48.1-25.
-
Liu TCY, Jiao JL, Xu XY, Liu XG, Deng SX, and Liu SH: Photobiomodulation: Phenomenology and its Mechanism, SPIE Proc. 2004; 5632: 185-191.
-
Hamblin MR, Demidova TN: Mechanisms of Low Level Light Therapy. SPIE Proc. 2006; 6140: 1-12.
-
Mester E, Szende B, Gartner P: Die Wirkung der Laserstrahlen auf den Haarwwuchs der Rad Biol Ther; 1967; 9/5: 621-626.
-
Mester E, Szende B, Tota JG: Effect of Laser on Hair Growth in Mice. Kiser! 1967; 19: 628-631.
-
Bernstein EF: Hair Growth Induced by Diode Laser Treatment. Dermatol Surg 2005; 31: 584-586.
-
Lolis MS and Marmur ES: Paradoxical Effects of Hair Removal Systems: a Review. J Cosmet Dermatol 2006; 5: 274-276.
-
Willey A, Torrontegui J., Azpiazu J, and Landa N: Hair Stimulation following Laser and Intense Pulsed Light Photo- epilation: Review of 543 Cases and Ways to Manage Lasers Surg Med 2007 ; 39: 297-301.
-
Avram MR, Leonard RT Jr, Epstein ES, Williams JL, and Bauman AJ: The current role of . laser/light sources in the treatment of male and female pattern hair loss. J Cosmet Laser Ther 2007; 9: 27-28.
-
Avram, MR and Rogers, NE: The use of low-level light for hair growth: part J Cosmet Laser Ther, 2009; 11: 110-117.
-
Stillman L: Reply to: The use of low-level light for hair growth: Part I. J Cosmet Laser Ther 2010; 12:
-
Bouzari N and Firooz AR: Lasers may induce terminal hair growth. Dermatol Surg 2006; 32:
-
Chung PS, Kim YC, Chung MS, Jung SO and RP-e CK: The Effect of Low-power Laser on the Murine Hair Growth. J Korean Soc Plastic Reconstruct Surg,
-
Leavitt M, Charles G, Heyman E, and Michaels D: HairMax LaserComb laser phototherapy device in the treatment of male androgenetic alopecia: A randomized, double-blind, sham device-controlled, multicentre trial. Clin Drug Invest 2009; 29: 283-292.
-
Yamazaki M, Miura Y, Tsuboi R, and Ogawa H: Linear polarized infrared irradiation using . Super Lizer is an effective treatment for multiple-type alopecia areata. Intl J Dermatol 2003; 42: 738-740,
-
Shukla S, Sahu K, Verma Y, Rao KD, Dube A, et al.: Effect of helium-neon laser irradiation on hair follicle growth cycle of Swiss albino mice. Skin Pharmacol and Physiol 2010; 23: 79··85.
-
Satino JL and Markou M: Hair Regrowth and Increased Hair Tensile Strength Using the HairMax LaserComb for Low-Level Laser Therapy. Intl J Cosmetic Surg Aesthet Dermatol 2003; 5: 113-117.
-
Trelles MA, Mayayo E, Cisneros JL. Tratamiento de la Alopecia Areata con laser Investigacion Y Clinica Laser 1984; 1:15 -17.
-
Lanzafame RJ, Blanche RR, Bodian AB, Chiacchierini RP, Fernandez-Obregon A, Kazmirek The growth of human scalp hair mediated by visible red light laser and LED sources in males. Lasers Surg Med 2013; 45(8):487-495.
-
Avci P, Gupta GK, Clark J, Wikonkal N, Hamblin MR. Low-Level Laser (Light) Therapy (LLLT) for Treatment of Hair Loss. Lasers Surg Med 20 l 4; 46(2):144-151.
-
Androgenetic Alopecia in Women, Vera H. Price, University of California San Francisco, Department of Dermatology, San Francisco, California, USA, l: vhprice@orca.ucsf.edu
-
Laser therapy: A review of its mechanism of action and potential medical applications; B. Tata, R.W. Waynant, Laser & Photonics Reviews. Jan 2011, Vol. 5, No. 10.1002/lpor.v5.1: 1-12
-
Irradiation at 634 nm releases nitric oxide from human monocytes, Ann Lindgård, Lillemor Mattsson Hultén, Lennart Svensson, Bassam Soussi, Lasers in Medical Science. Feb 2007, Vol. 22: 30-36
-
Laser Literature Watch, Photomedicine and Laser Surgery. Feb 2006, Vol. 24, No. 1: 74-99
-
Physiologic Rhythms Responding to Low-Level Electromagnetic and Mechanical Signals: The Joule Equivalence Principle, Luis A. Santana-Blank, Elizabeth Rodríguez-Santana, Photomedicine and Laser Surgery. August 2008: 405-406.
-
Low-Intensity Light Therapy: Exploring the Role of Redox Mechanisms, Joseph Tafur, Paul J. Mills, Photomedicine and Laser Surgery. August 2008: 323-328.
-
Intracellular signaling cascades following light irradiation, Shengnan Wu, Da Xing, Laser & Photonics Reviews. Apr 2013: n/a
-
Low-intensity laser irradiation at 660 nm stimulates cytochrome c oxidase in stressed fibroblast cells, Nicolette N. Houreld, Roland T. Masha, Heidi Abrahamse, Lasers in Surgery and Medicine. Jul 2012, Vol. 44, No. 10.1002/lsm.v44.5: 429-434
-
Laser Therapy in the Tissue Repair Process: A Literature Review, Jacqueline Pereira da Silva, Maéli Alves da Silva, Ana Paula Figueiredo Almeida, Império Lombardi Junior, Areolino Pena Matos, Photomedicine and Laser Surgery. Feb 2010, Vol. 28, No. 1: 17-21
-
The use of low-level light for hair growth: Part I, Marc R. Avram, Nicole E. Rogers, Journal of Cosmetic and Laser Therapy. Jun 2009, Vol. 11: 110-117
-
Biphasic Dose Response in Low Level Light therapy, Ying-Ying Huang, Aaron C.-H. Chen, James D. Carroll, Michael R. Hamblin, Dose-Response. Jan 2009, Vol. 7: 358-383
-
Utilizing electromagnetic radiation for hair growth: a critical review of phototrichogenesis. Kalia S, Lui H., Dermatol. Clin. 2013 Jan;31(1):193-200.
-
Update on the pathogenesis, genetics and medical treatment of patterned hair loss. Schweiger ES, Boychenko O, Bernstein RM., J Drugs Dermatol. 2010 Nov;9(11):1412-9.
-
Leavitt M, Charles G, Heyman E, Michaels D. HairMax LaserComb laser phototherapy device in the treatment of male androgenetic alopecia: A randomized, double-blind, sham device-controlled, multicenter trial. Clin Drug Investing. 2009;29(5):283-92
